Beyond Meat – The Evolving Role of Artificial Human Replicas in Medical Training and Simulation and the Impact on 3R
How modern phantoms and simulators are transforming ethical standards, replacing animal testing, and redefining realism in medical education and R&D.
Introduction
No, this is not another article about plant-based burgers.
Instead, it’s about something far more vital: the future of medical education and simulation. For centuries, cadavers and - more recently - animal models have served as the foundation for learning anatomy, practicing surgical techniques, and testing medical devices. These organic specimens have their rightful place in history, and even today, they remain indispensable in certain educational and research settings.
But medical science doesn’t stand still. As training becomes more technology-driven and ethically conscious, we’re entering a new era - one where artificial human replicas, also known as phantoms and simulators, are redefining how we teach, train, and test in healthcare.
This blog article takes a critical look at how these synthetic models are complementing - and in some cases, replacing - the traditional pillars of medical training. It explores how phantoms are making procedures safer to learn, easier to repeat, and more ethically sound. It also re-examines the 3R principles - Reduce, Refine, Replace - as a compass for more responsible innovation in medical simulation. While the 3R movement gained substantial traction over the last decade, its momentum seems to have slowed. We believe it’s time to refocus and ask: what lies beyond meat, and why should we go there?
Through historical insight, technical innovation, and practical examples, this article aims to give medical training facilities, skills labs, and device manufacturers a clear picture of the evolving role artificial models play - and the transformative impact they could have when implemented thoughtfully.
1. The Traditional Pillars: Cadavers and Animal Models
For many generations, medical training has been anchored by two foundational tools: human cadavers and animal models. Each offers unique benefits that have shaped the way healthcare professionals are educated and how new medical technologies are tested and refined.
Cadavers are the gold standard for anatomical education. They offer an irreplaceable opportunity to understand the human body in its full complexity - its variations, pathologies, and spatial relationships. Dissecting a human specimen allows trainees to appreciate the layered structure of tissues, the fragility of nerves, and the true three-dimensional nature of internal organs. For many, this is a rite of passage that lays the groundwork for surgical thinking and manual skill development.
Importantly, cadaver-based training also plays a critical role in shaping the emotional and psychological readiness of future physicians. For many students, it’s the first direct exposure to death in a clinical context. Working with a cadaver - seeing, touching, and even smelling human tissue in a state far removed from textbook diagrams - challenges trainees to confront the realities of mortality, decay, and physical vulnerability. This experience builds the professional composure necessary to perform under pressure and to manage difficult scenes without emotional paralysis. After all, no patient benefits from a physician who faints at the sight of blood.
Yet despite their unmatched realism, cadavers are limited in scope. They are static, non-perfused, and often lack the physiological feedback required to simulate real-life scenarios. Most are preserved through embalming techniques that alter tissue texture and color. Live-response training - such as practicing vascular access, catheter placement, or endoscopic navigation - is inherently restricted in this context.
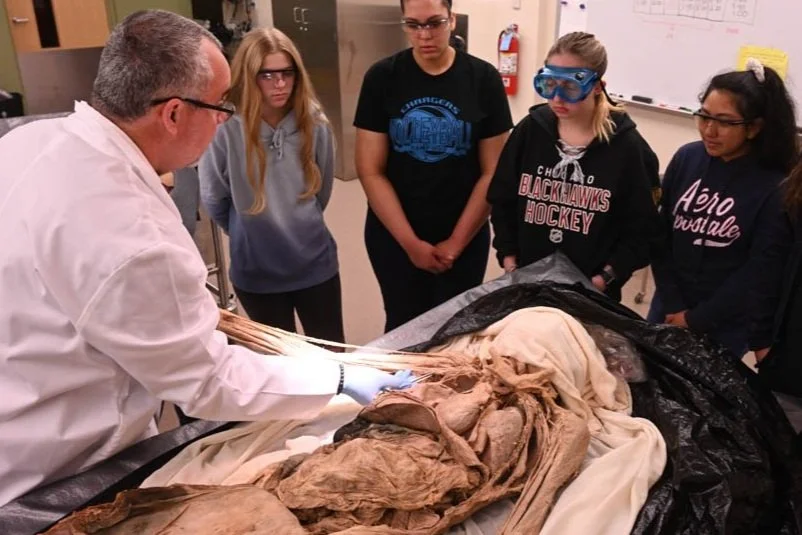
Cadaver Lab
Source: https://elginobserver.com/
Animal models, most commonly porcine, have been widely used as a workaround for those limitations. Their advantages are clear: they’re biologically “alive” during procedures, relatively easy to source, and subject to fewer regulatory constraints in many parts of the world. They offer a dynamic, reactive training environment - blood flow, breathing, cardiac activity - which is critical for certain types of interventions and device testing.
However, the anatomical differences between animals and humans are significant. Organ shape, tissue elasticity, and even vascular structure often do not align with human physiology. Devices optimized in porcine models may perform differently in human patients. And as medical ethics evolve, so too does the scrutiny of using sentient animals for educational purposes.
In addition, the use of porcine models specifically can pose cultural and religious challenges in certain regions - particularly in Muslim-majority countries, where handling pigs or pig-derived materials may be religiously prohibited. This can limit access to standard animal-based training protocols and complicate international training events or device demonstrations, reinforcing the need for culturally neutral alternatives like artificial simulators.
Still, these two tools - cadavers and animal models - remain deeply embedded in training culture. They continue to serve important roles, particularly in teaching foundational anatomy and exploring high-risk procedures. But as we’ll see in the following sections, their dominance is being challenged - not by ideology, but by innovation.
2. The Shift Toward 3R Principles
While cadavers and animal models have long been considered the cornerstones of hands-on medical education, growing ethical awareness and technological progress have pushed the field to explore more sustainable and humane alternatives. This shift is largely framed by the internationally recognized 3R principles: Reduce, Refine, and Replace the use of animals in scientific and educational contexts.
The concept of the 3Rs was first introduced in 1959 by British scientists William Russell and Rex Burch, in their landmark publication “The Principles of Humane Experimental Technique.” Their work laid the ethical and scientific foundation for improving the treatment of laboratory animals and introduced a systematic way of thinking about alternatives to animal use in research and training. Though originally focused on laboratory experiments, the principles have since expanded to include preclinical testing, biomedical research, and medical education.
Each of the three Rs addresses a different aspect of ethical improvement:
Reduce: Minimize the number of animals used to obtain valid data.
Refine: Modify procedures to reduce pain, stress, or suffering.
Replace: Substitute animal models with non-animal systems whenever feasible.
From the late 2000s through the 2010s, the 3R movement gained significant traction across Europe and parts of North America. Research grants were created to fund alternative technologies. Regulatory bodies began encouraging 3R-compatible test methods. Institutions formed ethics committees and animal welfare offices tasked with evaluating training protocols.
And yet, despite this strong momentum, the public and institutional focus on the 3Rs seems to have faded over the past few years. The topic has slowly slipped from the spotlight - perhaps a victim of shifting priorities or the false impression that the problem is “already solved.” From our perspective, this decline in attention is concerning. The availability of advanced alternatives has never been better - and yet they’re still underused in many areas of medical training and device testing.
This disconnect points to a deeper challenge: transitioning from ethical awareness to practical implementation. Artificial training models and simulators have evolved significantly - but only if institutions recognize their capabilities and make room for them in their programs can the 3Rs truly be realized. The following section explores how this implementation can be achieved - by complementing, not competing with, traditional tools.
3. Artificial Models: Complement, Not Conflict
A common misconception is that artificial human replicas aim to replace cadavers and animal models entirely. In reality, phantoms and simulators are best seen as complementary tools - ones that expand what’s possible in training and testing, especially when consistency, repeatability, and accessibility are essential.
Where cadavers teach anatomy and animal models simulate live responses, phantoms provide a controllable, ethical, and highly adaptable bridge between the two. They allow for repeated practice, rapid scenario resets, and freedom from biohazard restrictions - making them ideal for procedure-based training, product testing, and educational outreach.
One of the most overlooked advantages of artificial models is their public and portable usability. At HumanX Medical, we’ve previously critiqued a trend that has become far too common in the medical device industry: the use of bell peppers, gelatin blocks, or rubber tubing to demonstrate high-end devices in trade show booths. In our article on Pepperoscopy, we pointed out how inadequate these substitutes are for simulating anything even remotely human—let alone convincing a trained physician of a product’s real-life efficacy.
Artificial models can solve this problem elegantly. They allow companies and educators to present realistic, anatomically accurate procedures in public settings without compromising ethics, realism, or professionalism.
This is particularly relevant for fields like gynecology and urology, where many procedures are highly intimate or invasive. Simulating these interventions - be it an endoscopic evaluation, catheterization, or a pelvic examination - is virtually impossible to do live at a conference or open training session. Human actors are inappropriate, and cadaveric options are impractical or legally restricted in such environments. Phantoms offer a solution that’s both dignified and didactically sound, making them indispensable for mobile skills training units, exhibition booths, or workshops with mixed experience levels.
One case that highlights this perfectly is a project we at HumanX developed in collaboration with a biotech company specializing in stem-cell treatment for anal fistulas, a debilitating condition often associated with Crohn’s disease. To train physicians on the precise application technique of the stem-cell solution, we created a patient-specific anatomical training model: a female pelvis in high lithotomy position, accurately replicating the typical external openings and internal tracts of anal fistulas. This model allowed for hands-on, repeatable training - without ethical barriers, without needing a clinical setting, and without the anatomical inaccuracies of an animal surrogate. Neither cadavers nor animals would have been suitable for such a task. But with the right phantom, training was safe, precise, and anatomically faithful.
Training models for practicing stem-cell treatment for anal fistulas.
Source: HumanX Medical
Moreover, many artificial models today are modular, allowing users to open and inspect internal structures, replace components, or simulate various complications. Some even include dynamic functions like pulsatile blood flow, responsive valves, or fluid feedback systems - all designed to mimic real-world anatomy and physiology more closely than ever before.
This is not about choosing one tool over another - it’s about combining the best features of each. Cadavers teach structure, animals offer dynamics, and phantoms deliver repeatability, safety, and accessibility. Together, they form a robust training ecosystem, one in which artificial models are no longer an afterthought but an essential pillar.
4. Breaking the Stereotypes
When many people hear the term “medical phantom” or “simulator,” they still imagine something stiff, simplistic, and clinical - perhaps a glossy plastic mannequin with jointed limbs and vacant eyes, like those used in basic CPR training or high school science classrooms. This outdated image couldn’t be further from the current reality.
Today’s phantoms are sophisticated, anatomically detailed, and functionally dynamic. They are no longer generic shells for practicing surface-level procedures but highly engineered tools that simulate real human anatomy - and, increasingly, real pathology - with astonishing precision.
One of the major drivers behind this transformation is the emergence of advanced materials.
Hydrogels - soft, water-rich polymer networks - are now widely used to replicate the consistency and elasticity of soft human tissue. Their mechanical properties can be finely tuned to resemble everything from mucosa to muscle, making them ideal for ultrasound training, puncture feedback, or endoscopic navigation. Some hydrogel variants are even transparent or radiopaque, enabling compatibility with imaging systems like fluoroscopy, ultrasound, or CT.
Soft silicones and medical-grade elastomers bring durability to the table. When used in layered constructions or combined with different infill geometries, these materials can mimic the resistance and compliance of organs, vessels, and connective tissue. They can be cut, sutured, or injected - just like their biological counterparts.
3D printing has added another revolution. Not only can we now fabricate patient-specific models from CT or MRI scans, but we can also print with multi-material capabilities, creating variable softness within the same structure. That means a single model might have a flexible airway, a firm tracheal ring, and a transparent larynx - all fused in one print job.
3D printed anatomical model based on a 3D scan of a human cadaver.
Source: Erler - Zimmer
These innovations are not just about realism - they’re about enabling precision, repetition, and reproducibility. A simulator can be designed to replicate a rare malformation or a specific procedural challenge. It can be printed again and again, exactly the same each time - something no cadaver or animal model can offer.
And yet, despite this progress, skepticism remains in some quarters. We’ve encountered professionals who still believe phantoms are only good for “dry runs,” or that plastic materials could never feel lifelike enough for surgical practice. These assumptions are outdated. The reality is that many of today’s simulators offer a tactile and visual experience that closely approximates human tissue, often more reliably than what’s found in a preserved cadaver.
By confronting these stereotypes head-on, we can open the door to broader adoption - not just in high-tech labs, but in everyday training rooms, device demonstrations, and global educational initiatives.
5. Why the Hesitation?
If artificial human replicas are so advanced, so customizable, and so clearly aligned with ethical and practical goals - why aren’t they used more widely?
The answer is a mix of perception, tradition, and infrastructure.
One of the most persistent doubts about phantoms and simulators stems from early-generation models. Those who encountered rigid plastic torsos or unrealistic silicone limbs in the past may have formed lasting impressions - believing that all simulators are inherently less realistic than organic tissue. In many cases, this belief persists even among decision-makers who haven’t seen or handled a modern phantom firsthand.
There’s also the issue of perceived cost. A well-designed simulator - especially one tailored to a specific procedure or pathology - may appear expensive at first glance. However, this perspective often ignores the full picture. Artificial models are reusable, transportable, and low-maintenance. They don’t require refrigeration, embalming, biohazard disposal, or post-use sanitization. Over time, they often prove more economical than cadavers or animal-based training setups, especially when amortized across multiple sessions or locations.
Then there’s the infrastructure challenge. Traditional hands-on training often depends on WetLabs - dedicated facilities equipped to host cadaveric or animal-based sessions. These labs are limited in number, geographically concentrated, and often booked months in advance. Organizing a WetLab session can involve securing ethical approvals, sourcing and prepping specimens, and coordinating technical staff and equipment.
The logistical burden becomes even heavier when training is meant for multiple team members or international participants. Flights, hotels, per diems, and administrative overhead add up quickly - often far exceeding the cost of the actual training session. And even when all these resources are mobilized, specimen availability is not guaranteed, especially when specific anatomy or pathology is required.
In contrast, phantoms can travel. They can be shipped to hospitals, industry events, or in-house training facilities. They can be used repeatedly, even back-to-back in rotating sessions. They remove bioethical roadblocks and significantly reduce organizational complexity - turning a weeks-long planning effort into a plug-and-play experience.
And yet, adoption still lags. Why? Because it often requires a mindset shift: moving away from what has always been done, toward what could be done better. Institutions and manufacturers alike may need support in evaluating, testing, and integrating artificial models into their programs - but once that step is taken, the benefits become immediately clear.
6. Case for Broader Adoption in R&D
Artificial human replicas aren’t just useful for training - they also hold enormous untapped potential in research and development, especially within medical device innovation. In fact, many of the advantages phantoms bring to simulation-based learning apply equally to product design, testing, and validation.
In traditional preclinical workflows, animal models have long been used to approximate human anatomy and function. But this comes with limitations: high variability, anatomical mismatch, regulatory hurdles, and ethical concerns. Even when used appropriately, animal data often fails to predict device behavior in the human body with sufficient accuracy - especially for procedures requiring precise spatial control, like catheter navigation, valve deployment, or targeted drug delivery.
This is where phantoms offer distinct advantages:
Repeatability: A phantom with known internal geometry and mechanical properties can be used across multiple R&D sessions, ensuring consistent conditions for every test. This is especially valuable when comparing device iterations or handling techniques.
Standardization: Custom-designed models can match the exact vessel diameter, branching angle, or pathology relevant to the product being developed - eliminating confounding anatomical differences found in animal or cadaver specimens.
Realistic Feedback: Modern simulators can mimic the tactile, mechanical, and flow conditions found in human tissue. Some include features like pulsatile circulation, temperature-controlled environments, or responsive valves to allow for more lifelike testing scenarios.
Imaging Compatibility: High-end phantoms can be designed for use under fluoroscopy, ultrasound, MRI, or CT, allowing real-time visualization of device behavior in a controlled environment - without radiation exposure or biological decay.
Regulatory Support: Simulators can support early-stage validation and verification protocols by offering reproducible data. Regulatory agencies are increasingly open to alternative testing methods when justified with sound methodology.
At HumanX Medical, we’ve seen these benefits firsthand. Whether it's a catheter manufacturer simulating deployment in an aneurysm model, or a biotech company testing a new injection protocol inside a vascular phantom, the ability to isolate variables and iterate quickly can reduce development time, cut costs, and enhance product safety before clinical trials even begin.
Yet despite these advantages, simulators are still underutilized in many R&D departments. The reasons often echo those in clinical training: lack of awareness, outdated perceptions, and internal inertia. But with the right collaboration between simulator developers, engineers, and clinicians, phantoms can become a central pillar of evidence-based, ethically responsible device development.
7. A Glimpse into the Future – Neonatal Simulation Without Compromise
One of the most ethically and technically challenging areas in medical simulation is the neonatal field. Procedures involving newborns demand extreme precision, gentle handling, and specialized instrumentation. And yet, training and product development for this age group remains deeply constrained by the lack of suitable models.
In the context of this article, the need for realistic, ethical, and anatomically faithful solutions is especially urgent in the field of neonatal simulation. Traditional methods - often involving rabbits or piglets - fall short due to anatomical mismatch, ethical concerns, and limited availability. Cadaveric options are virtually nonexistent, and the few animal-based models that do exist rarely offer the procedural fidelity required for training or device development.
Recognizing these challenges, a growing number of developers - including HumanX Medical - are actively exploring new ways to replicate the unique anatomical conditions of newborn patients. These efforts aim to support surgical training, product demonstration, and medical innovation without relying on sentient animal models or ethically restricted alternatives. Although many of these projects are still under development, they represent an important step toward refining and replacing outdated approaches in one of medicine’s most delicate and demanding domains.
Nothing can replace it - training system for neonatal surgeries
Source: HumanX Medical
These ongoing initiatives underscore the evolving role of artificial replicas - not just as tools of convenience, but as solutions that meet ethical, educational, and clinical demands head-on, even in areas where traditional methods offer no viable alternative.
Conclusion: Beyond Meat, Beyond Limits
Medical education and simulation are evolving. What once depended solely on cadavers and animal models is now being transformed by technology, ethics, and a growing demand for accessible, repeatable, and anatomically realistic training environments. Artificial human replicas - phantoms and simulators - are no longer fringe tools or emergency substitutes. They are, increasingly, the standard of choice for high-quality, high-integrity simulation and R&D.
This shift is not about rejecting the past. Cadavers still provide unmatched opportunities for learning human anatomy, and in certain cases, animal models may continue to serve a narrow but necessary function. But as this article has shown, the limitations, ethical challenges, and logistical hurdles of traditional methods are becoming harder to justify - especially when powerful alternatives are available.
Whether it’s improving procedural confidence, accelerating product development, reducing reliance on animals, or democratizing access to realistic training, artificial models are enabling new levels of precision, responsibility, and innovation. And nowhere is this more critical than in fields where traditional tools fall short - such as pediatric and neonatal simulation.
Now is the time to reignite the 3R conversation. To move from principle to practice. To invest in solutions that are not only effective but scalable, humane, and future-ready.
Because going beyond meat is not just about materials - it’s about mindset.